Complete AI and RPA-enabled RCM Healthcare Solutions
Streamlined solutions for maximizing revenue and minimizing hassle using cutting-edge technology
 Get Started Today
Get Started TodayRCM services to boost your Revenue
RCM management services that increase the health of a practice's revenue

The healthcare sector loses billions of dollars annually because of poor medical billing revenue cycle management (RCM). Don't let this happen to your organization. Secure its cash flow with RCM healthcare solutions from Plutus Health Inc.
As one of the leading RCM providers in the country, Plutus Health Inc. offers complete healthcare RCM services.

Claim Scrubbing and Submission
The number of denied or rejected claims is reduced drastically when you incorporate successful claims scrubbing that detects and eliminates errors in billing codes before submission.

Account Receivables Management & Follow-up
Account Receivables (or AR) is money owed to the provider based on the different patient accounts for services rendered. AR is payable by insurance firms and patients.

Patient Registration
Your registration process will capture your patients' information, including insurance information. Ensuring an optimized process ensures you get paid faster for services rendered.

Patient Statements
One of the fastest ways to ensure positive cash flow is to improve your process that generates and mails patient statements. Expedite patient payment collections with automated processes.

Medical Coding
Medical coding converts medical diagnoses, dealings, and reports into a collective list of assigned medical code numbering. Appropriate medical coding helps to get reimbursements for all the services rendered.

Medical Billing Company
Plutus Health offers outsourced medical billing services that increase the health of a practice's revenue. Our team is ready to help you.

Charge Entry
Charge entry is the most critical feature of the medical billing cycle where the claims are actually created. Leverage AI to post accurate charges and reduce your claim denials.

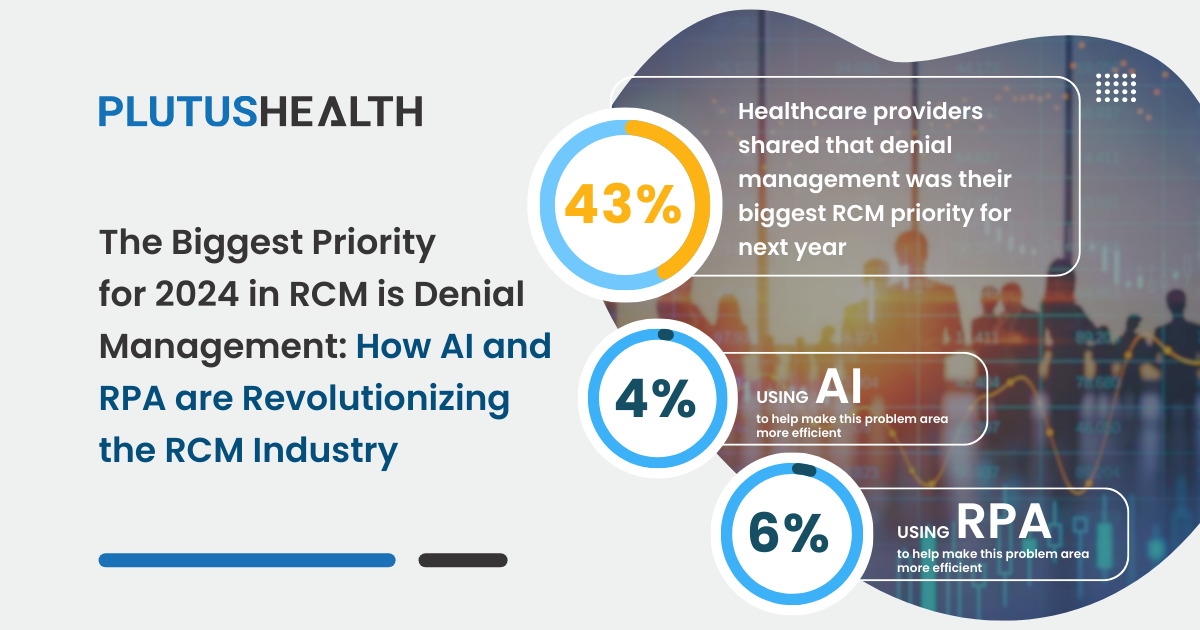
Denial Management Appeals
Insurance companies deny many claims by patients or providers due to incomplete claim forms, wrong diagnosis codes, incorrect modifiers, and more.

Insurance Eligibility and Benefits Verification Services
Insurance eligibility verification is an important process wherein a provider's practice or healthcare facility checks into a patient's insurance coverage to learn what insurance services or treatments will cover to offer better consultation & care.

Provider Enrollment & Credentialing
Provider enrollment & credentialing is a detailed process that reviews a provider's qualifications and career history, including education, training, residency and licenses, and specialty certificates.

Claim Scrubbing and Submission
The number of denied or rejected claims is reduced drastically when you incorporate successful claims scrubbing that detects and eliminates errors in billing codes before submission.

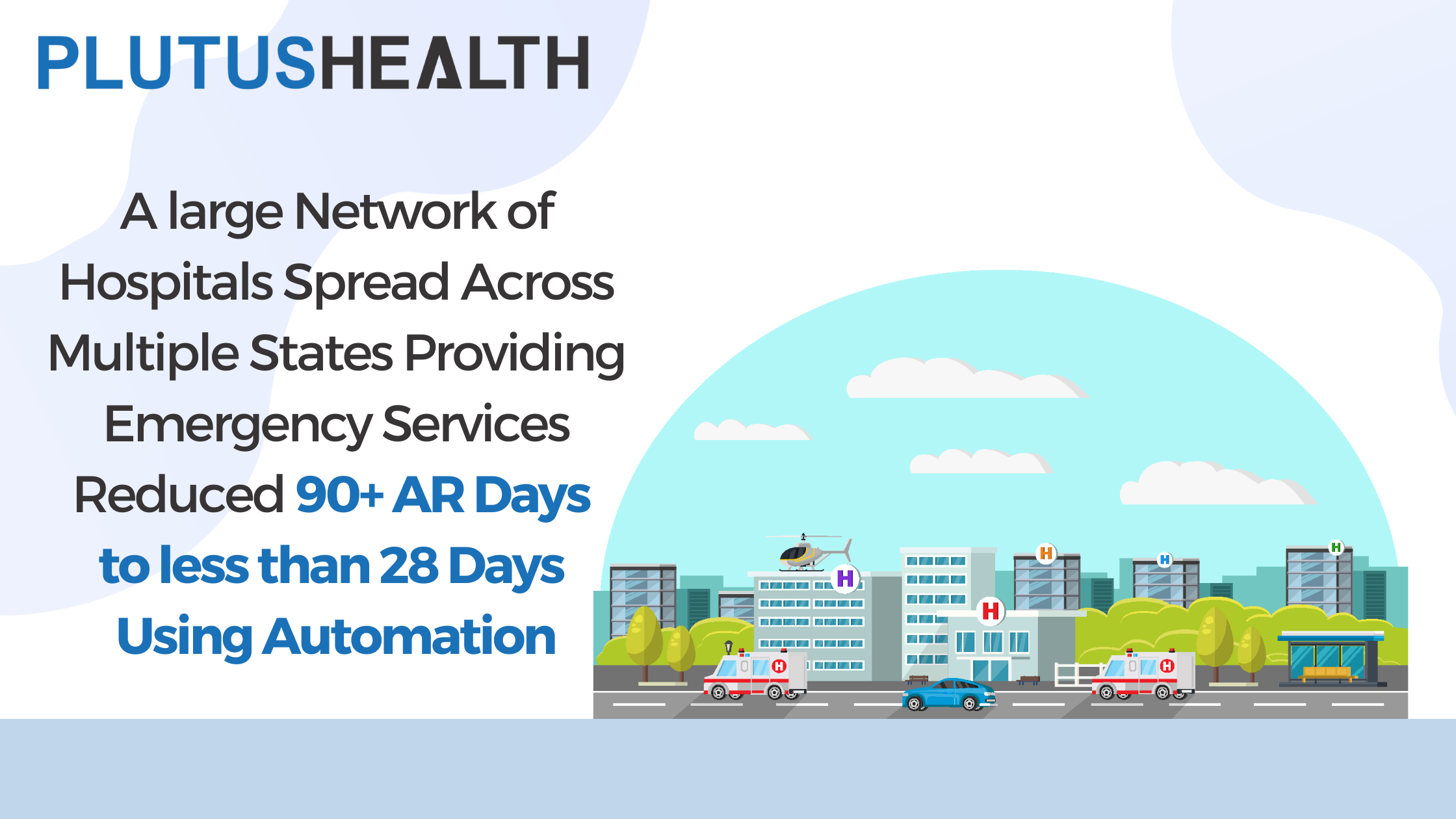
Account Receivables Management & Follow-up
Account Receivables (or AR) is money owed to the provider based on the different patient accounts for services rendered. AR is payable by insurance firms and patients.

Patient Registration
Your registration process will capture your patients' information, including insurance information. Ensuring an optimized process ensures you get paid faster for services rendered.

Patient Statements
One of the fastest ways to ensure positive cash flow is to improve your process that generates and mails patient statements. Expedite patient payment collections with automated processes.

Medical Coding
Insurance eligibility verification is an important process wherein a provider's practice or healthcare facility checks into a patient's insurance coverage to learn what insurance services or treatments will cover to offer better consultation & care.

Medical Billing Company
Plutus Health offers outsourced medical billing services that increase the health of a practice's revenue. Our team is ready to help you.

Charge Entry
Charge entry is the most critical feature of the medical billing cycle where the claims are actually created. Leverage AI to post accurate charges and reduce your claim denials.

Denial Management Appeals
Insurance companies deny many claims by patients or providers due to incomplete claim forms, wrong diagnosis codes, incorrect modifiers, and more.

Insurance Eligibility and Benefits Verification Services
Insurance eligibility verification is an important process wherein a provider's practice or healthcare facility checks into a patient's insurance coverage to learn what insurance services or treatments will cover to offer better consultation & care.

Provider Enrollment & Credentialing
Provider enrollment & credentialing is a detailed process that reviews a provider's qualifications and career history, including education, training, residency and licenses, and specialty certificates.

Claim Scrubbing and Submission
The number of denied or rejected claims is reduced drastically when you incorporate successful claims scrubbing that detects and eliminates errors in billing codes before submission.

Account Receivables Management & Follow-up
Account Receivables (or AR) is money owed to the provider based on the different patient accounts for services rendered. AR is payable by insurance firms and patients.

Patient Registration
Your registration process will capture your patients' information, including insurance information. Ensuring an optimized process ensures you get paid faster for services rendered.

Patient Statements
One of the fastest ways to ensure positive cash flow is to improve your process that generates and mails patient statements. Expedite patient payment collections with automated processes.

Medical Coding
Medical coding converts medical diagnoses, dealings, and reports into a collective list of assigned medical code numbering. Appropriate medical coding helps to get reimbursements for all the services rendered.

Medical Billing Company
Plutus Health offers outsourced medical billing services that increase the health of a practice's revenue. Our team is ready to help you.

Charge Entry
Charge entry is the most critical feature of the medical billing cycle where the claims are actually created. Leverage AI to post accurate charges and reduce your claim denials.
.webp)
Denial Management Appeals
Insurance companies deny many claims by patients or providers due to incomplete claim forms, wrong diagnosis codes, incorrect modifiers, and more.

Insurance Eligibility and Benefits Verification Services
Insurance eligibility verification is an important process wherein a provider's practice or healthcare facility checks into a patient's insurance coverage to learn what insurance services or treatments will cover to offer better consultation & care.

Provider Enrollment & Credentialing
Provider enrollment & credentialing is a detailed process that reviews a provider's qualifications and career history, including education, training, residency and licenses, and specialty certificates.
Combination of technology and expertise to help you grow
Plutus Health has a team of experts that leverage cutting-edge technology to provide RCM services. Our revenue cycle management solutions help you streamline your cash flow and seamlessly grow your practice.
Intelligent healthcare revenue cycle management solutions to help you succeed

Plutus Health provides tech-enabled RCM services and solutions to help healthcare providers optimize revenue, reduce costs, increase efficiency, and accelerate cash flow.
We have developed deep healthcare RCM expertise and leverage AI, ML, & RPA to automate RPA processes and reduce errors to <1%. We provide all the resources you need to scale your practice, combat RCM challenges, and achieve your financial goals.
Our clients enjoy custom strategies tailored to each practice or lab's unique revenue flow challenges. Plus, we're so committed to helping our clients save money that we always offer the option to work with a client's existing software! Our dedicated team is ready to help you create a revenue growth action plan with automated, optimized processes.
Get Started NowTop Advantages of Outsourcing Your RCM
Practices that outsource their RCM tasks experience:
- Increased revenue and clean claims due to certified coders and claim scrubbing process
- Faster reversals by team working on denied or rejected claims
- Maximized revenue flow due to the cost-effective nature of outsourcing
- Reduced debt, denials, operational costs, and expenditure
- Round-the-clock services and excellent TAT delivery
- Advanced automation and technological advantages that speed up the process without risk of error










.jpg)
.jpg)
.jpg)







