AR Management in Healthcare RCM: Tips, Importance, and Benefits
Healthcare organizations lose 5-15% of their annual revenue due to improper accounts receivable management. The MGMA (Medical Group Management Association) survey found that the average A/R (Accounts Receivable) percentage over 120 days is 13.54%. This blog will give you information about tips, benefits, and the importance of AR management.
In this blog:
- What is AR management in healthcare RCM?
- Why is AR management important in the RCM Cycle?
- What are the three stages of AR management?
- Tips for efficient AR management
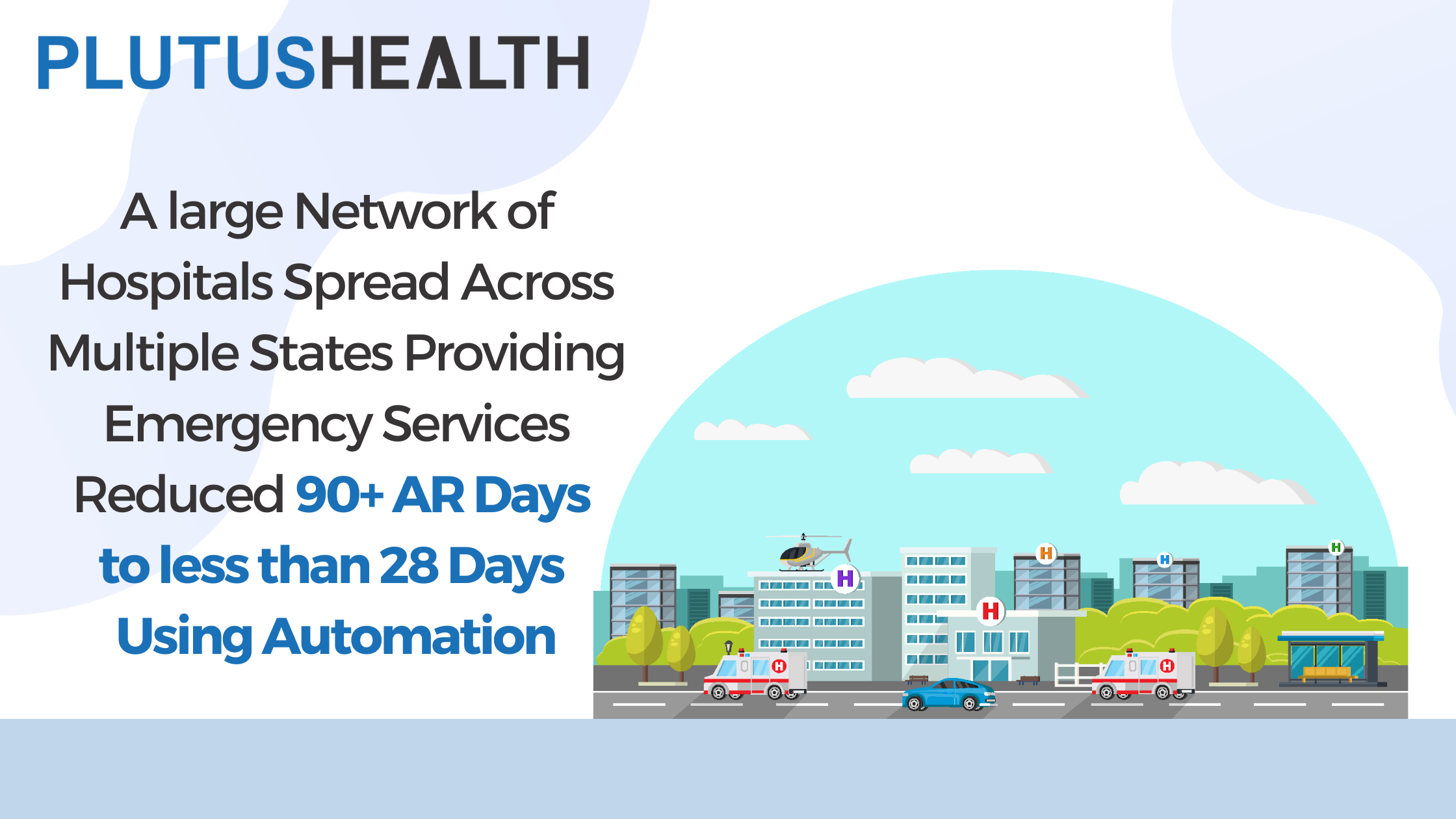
Accounts receivable (AR) in healthcare RCM refers to tracking and collecting payments from insurance companies and patients for healthcare providers' services. If a healthcare organization has an average AR of 60 days, it takes 60 days to collect payment from insurance companies and patients. AR days for any healthcare organization should be below 25 days.
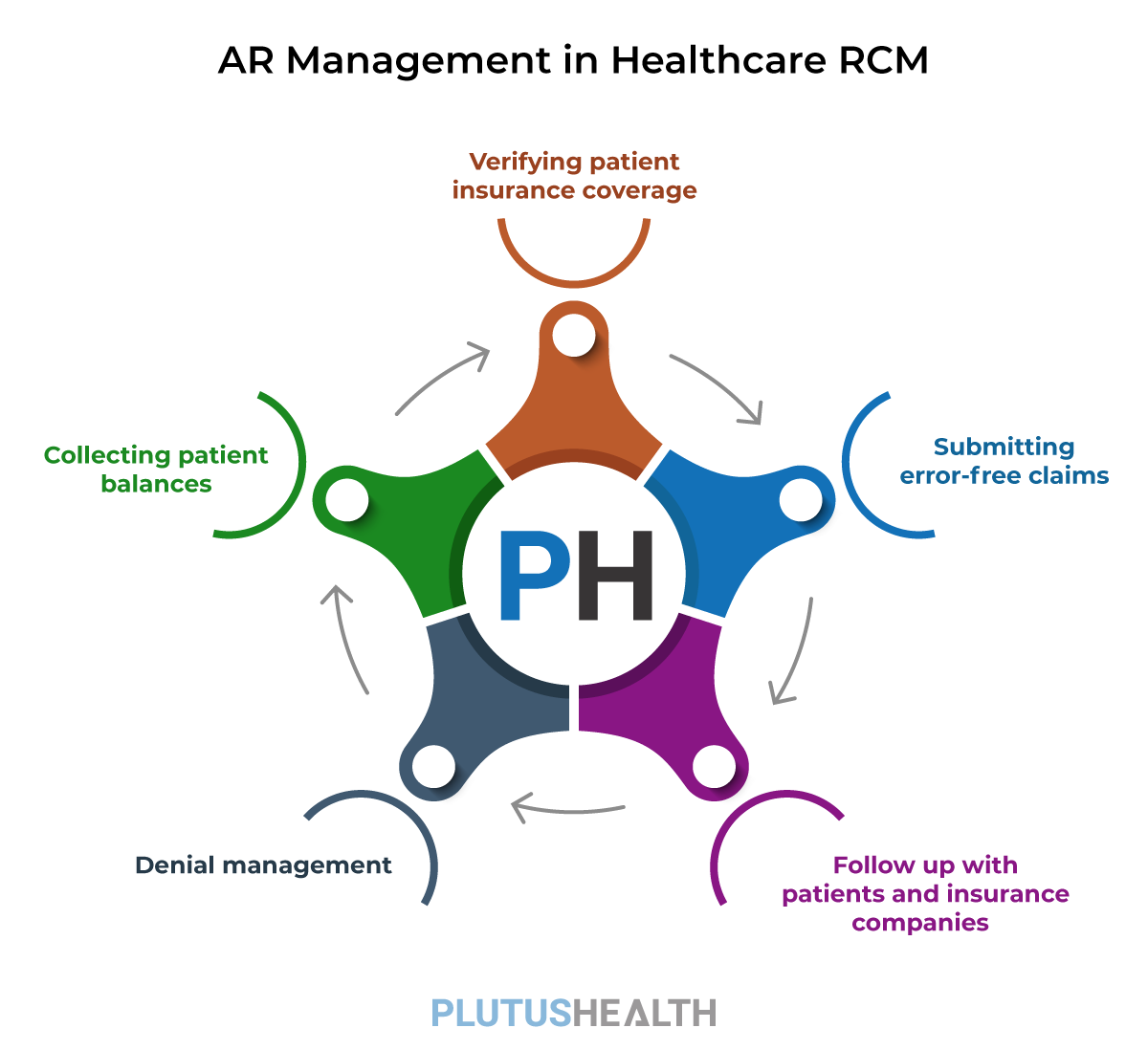
If the healthcare providers don't get payments for months or the payment gets constantly delayed, then it is called aging AR. Aging AR impacts the financial health of an organization. AR management tracks the entire revenue cycle process, from verifying patient insurance coverage, submitting claims, and following up on unpaid claims to managing denials and collecting patient balances.
"Efficient AR management is vital to streamline cash flow, reducing operating costs, and maximizing reimbursement," said Balaji Ramani, Vice President of RCM research & analyst, Plutus Health
Verifying patient insurance coverage
Healthcare providers must verify patient insurance coverage before offering healthcare services to patients. Insurance verification assures healthcare providers that they will get reimbursed for their services. Even the patients can understand their out-of-pocket costs and insurance coverage. In a survey, American Hospital Association found that the hospitals provided $41.6 billion in uncompensated care.
Submitting error-free claims
Healthcare organizations pay an average of $15- $20 per claim to manage and submit claims. It is important to appropriately submit these claims for the first time as denials increase this cost to 3X. Healthcare providers who submit error-free claims have seen a significant increase in cash flow. Claim submission is an important step in healthcare RCM. It requires experienced medical billers and coders to submit clean claims.
Follow up with patients and insurance companies
There are multiple follow-ups required to collect payments from patients or insurance companies. Timely follow-up on AR is important for uninterrupted cash flow. Healthcare providers must constantly connect with patients and insurance companies to reduce their AR. Good relations with payers and patients are the key to seamlessly managing AR. Healthcare providers should be prompt with their follow-ups to keep their cash flow healthy.
Denial management
Identifying the root cause of denials is vital for effective AR management. The claim denials can be either due to coding or billing errors. Denial management requires an experienced team to analyze the reason for denials and immediately re-submit the clean claim. Healthcare providers must also do a denial trend analysis to detect the patterns and eradicate the most common denial reasons.
Collecting patient balances
A major chunk of revenue for a healthcare organization is dependent on patients. Collecting patient payments is the most crucial yet difficult task while managing your AR. A survey by MGMA found that patient balance collection is only around 57% if they are billed after the services rendered. Healthcare providers can use patient collection tools like AnodynePay to engage patients and collect payments faster.
Periodic reports and audits
Reporting, analytics, and auditing are a few of the top qualities an AR management team must have. Audits help healthcare providers to access risks and detect problems. The reports generated from the audits aid in segregating outstanding payments, aging AR, and more. The AR team should analyze the cause of the delay and ensure there are no further denials.
Account receivable management is important in the RCM cycle as the organization's financial health depends on it. Right from when the patient books an appointment until the healthcare provider receives the payment, AR management plays a significant role in streamlining the process. Here are the other reasons why AR management is important
Streamlined cash flow
AR management is critical for cash flow management. Steady cash flow is the backbone of any healthcare organization. Steady cash flow is especially important for healthcare providers as they must pay on time for supplies, equipment, and staff salaries. Effective AR management can ensure the cash to cover expenses and invest in growth opportunities.
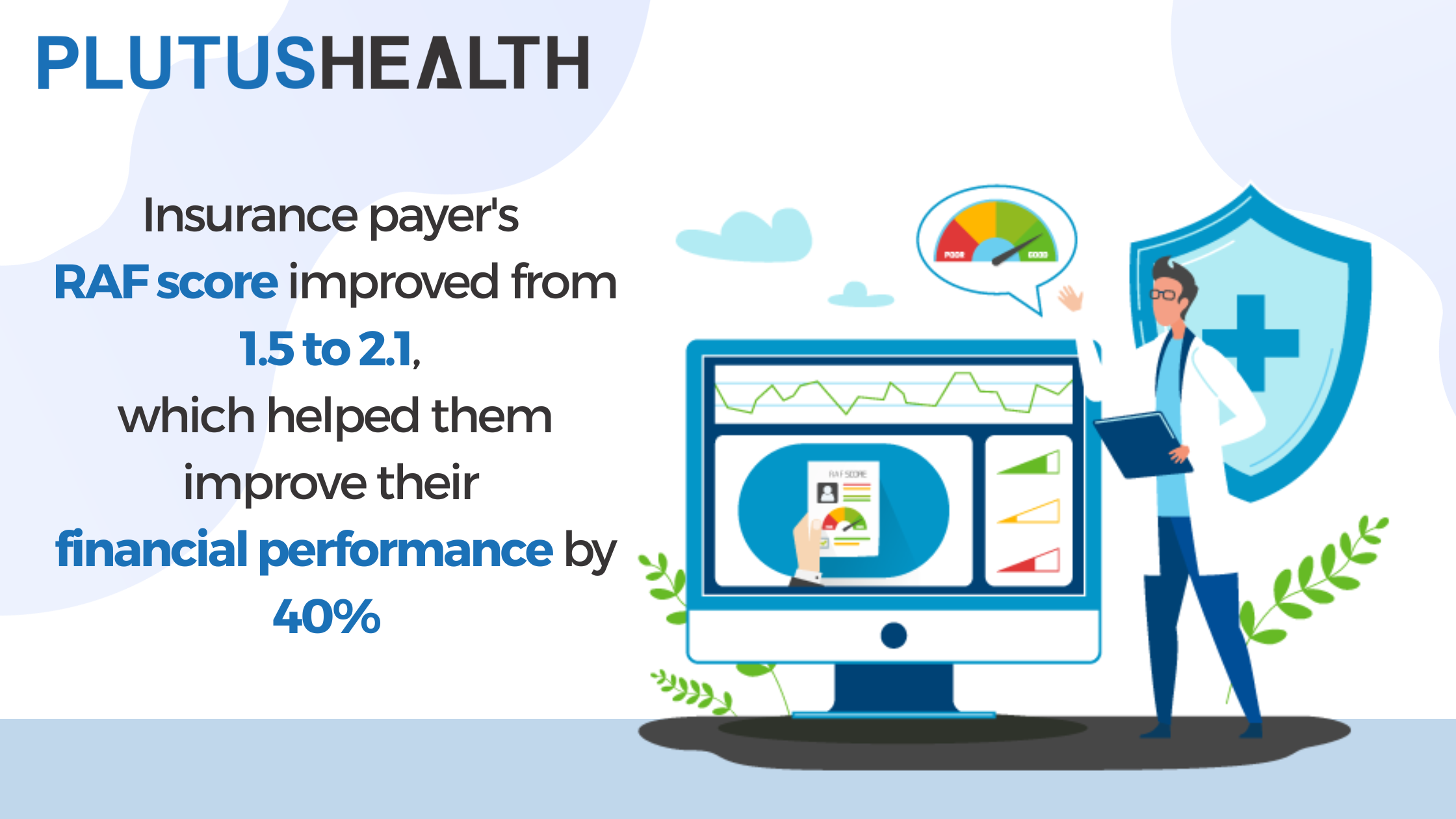
Revenue optimization
By managing AR effectively, healthcare organizations can increase their revenue and profitability. AR is also critical for revenue optimization. Effective AR management ensures all eligible claims are paid in full and on time. AR management can also help prevent revenue leakage and minimize write-offs. Healthcare organizations with effective AR management have seen denials below 5%.
Increase patient satisfaction
Timely and accurate billing is the key to patient satisfaction. 69% of patients said they would switch healthcare providers for a better experience. Patients demand clear and accurate bills along with a seamless payment option. They want answers to their questions promptly. Healthcare providers can enhance the patient experience with effective AR management.
Stay compliant
Compliance is crucial for healthcare organizations, as non-compliance can lead to fines, legal fees, and reputational damage. Accounts receivable management experts know all the rules and documents healthcare organizations demand. It seamlessly reduces penalties and audit risks. AR management also ensures that healthcare providers submit clean claims.
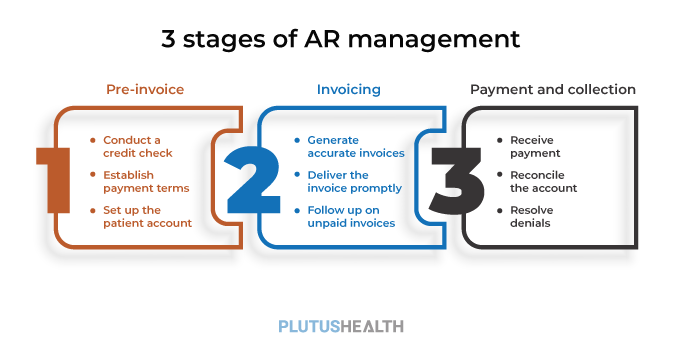
There are three stages of AR management that healthcare providers should be aware of. Let's discuss each stage in detail.
Stage 1: Pre-invoice
The pre-invoice stage is the first stage of AR management. It involves setting up the payer/patient’s account, verifying the patient's creditworthiness, and establishing payment terms. The pre-invoice stage is vital as it sets the foundation for the entire AR management process. During this stage, businesses should:
- Conduct a credit check: Before giving services to a patient, it's essential to verify their creditworthiness. A credit check can provide insight into the patient's payment history, credit score, and financial stability.
- Establish payment terms: Many patients want a cost estimation before starting medical treatment. Once the credit check is complete, healthcare providers should establish payment terms with patients/payers. Payment terms can vary depending on the patient insurance coverage and creditworthiness.
- Set up the patient account: Once the payment terms get established, healthcare providers should set up the patient account. It includes gathering the patient's contact information, billing address, and payment preferences.
Stage 2: Invoicing
The invoicing stage is the second stage of AR management. It involves creating and sending invoices to patients and payers for services. This stage is vital because it establishes a payment expectation with the payers and patients. During this stage, healthcare providers should:
- Generate accurate invoices: On average, healthcare providers receive their reimbursement after 60-120 days. Ensuring that the invoice is accurate, including the correct medical codes and service descriptions is essential. Inaccurate invoices can lead to payment delays.
- Deliver the invoice promptly: Delivering the invoice promptly can help ensure timely payment. Healthcare should consider electronic billing to speed up delivery.
- Follow up on unpaid invoices: If the patients or payers do not pay the amount within the established payment terms, it's essential to follow up promptly. Follow-up can involve sending a reminder email or making a phone call.
Stage 3: Payment and Collection
The payment and collection stage is the final stage of AR management. It involves collecting payments from the patients/payers and resolving any payment discrepancies. During this stage, healthcare providers should:
- Receive payment: Once the payer/patient makes a payment, it's essential to record the payment accurately in the accounting system.
- Reconcile the account: Reconciling the account can help identify any errors in the payment received.
- Resolve denials: 30% of claims submitted by healthcare providers are denied. If there are any payment denials, it's essential to resolve them promptly. It can involve identifying the cause of denials and appealing for payment.
Efficient AR management is the backbone of the healthcare RCM process. It minimizes write-offs and ensures timely payments. Here are tips for efficient AR management.
"AR management demands an in-depth understanding of RCM processes, data, and workflow. You should be able to thoroughly analyze data and identify the patterns that increase your AR."
Verify patient insurance eligibility
Healthcare providers should verify patient insurance eligibility before providing any healthcare services. Insurance verification reduces claim denials and rejections, resulting in timely payments. It also ensures that the correct insurance information gets captured during registration.
Accurate coding
Accurate coding ensures timely and accurate payments. Coding errors can lead to claim denials that result in delayed payments. Healthcare providers should have a certified coding team that is up to date with the latest coding guidelines and regulations.
Timely submission of claims
It is important to establish a system to track claims. Timely submission of claims helps healthcare providers to receive payments promptly. A proper system ensures that they submit claims within the specified timeframe. Delayed claim submission can slower payments and increase denials.
Follow-up on outstanding claims
Regular follow-up on outstanding claims is essential to get timely payments. It is important to establish a system to track outstanding claims and follow up on them regularly. Timely follow-up can help reduce the number of denials and write-offs.
Monitor denials and appeals
Monitoring denials and appeals is essential to identify trends and patterns in claim denials. Healthcare providers should track denials and appeals. It helps to analyze the data and identify the root cause of denials. Monitoring ultimately helps reduce denials and improve the overall RCM process efficiency.
Establish payment plans
Offering payment plans to patients improves collections. Establishing a system to manage payment plans and implement them correctly is important.
Train staff
Proper training of staff is essential for efficient AR management. Providing regular training to staff on the latest coding guidelines, regulations, and best practices helps improve the accuracy of the AR management process.
What AR management process should you outsource?
The decision to outsource AR management processes in healthcare RCM can depend on several factors, such as the organization's size, the complexity of the revenue cycle, and the expertise of the in-house staff. However, there are certain AR management processes that healthcare organizations commonly outsource.
Healthcare organizations must carefully evaluate their options when considering outsourcing AR management processes. Factors to consider include:
Efficient AR management outsourcing
Healthcare providers have found that outsourcing AR management has made them effective and efficient.
Plutus Health has 15+ years of experience in healthcare RCM. Our team of certified and experienced professionals thoroughly knows the AR management process. Our team implements strategies and processes that ensure timely and accurate reimbursement from insurance companies and patients.
Our AR management services include verifying patient eligibility and benefits, submitting claims on time, following up on unpaid claims, and more. We ensure prompt payment. Click here to schedule a call with our AR management experts.