Decoding the 2026 OPPS/ASC Proposed Rule: What CFOs Need to Know About Payment Shifts
Centers for Medicare & Medicaid Services (CMS) has published the 2026 Proposed Rule for the Hospital Outpatient Prospective Payment System (OPPS) and Ambulatory Surgical Centers (ASCs). This rule indicates significant changes in how ASCs will be reimbursed and function. These initiatives create new revenue growth opportunities for agencies along with new operational issues. ASC CFOs and revenue cycle executives need to comprehend these proposals so they can adjust their financial plans and preserve margins for years beyond.
ASC Payment Rates: A Modest Increase with Strategic Implications
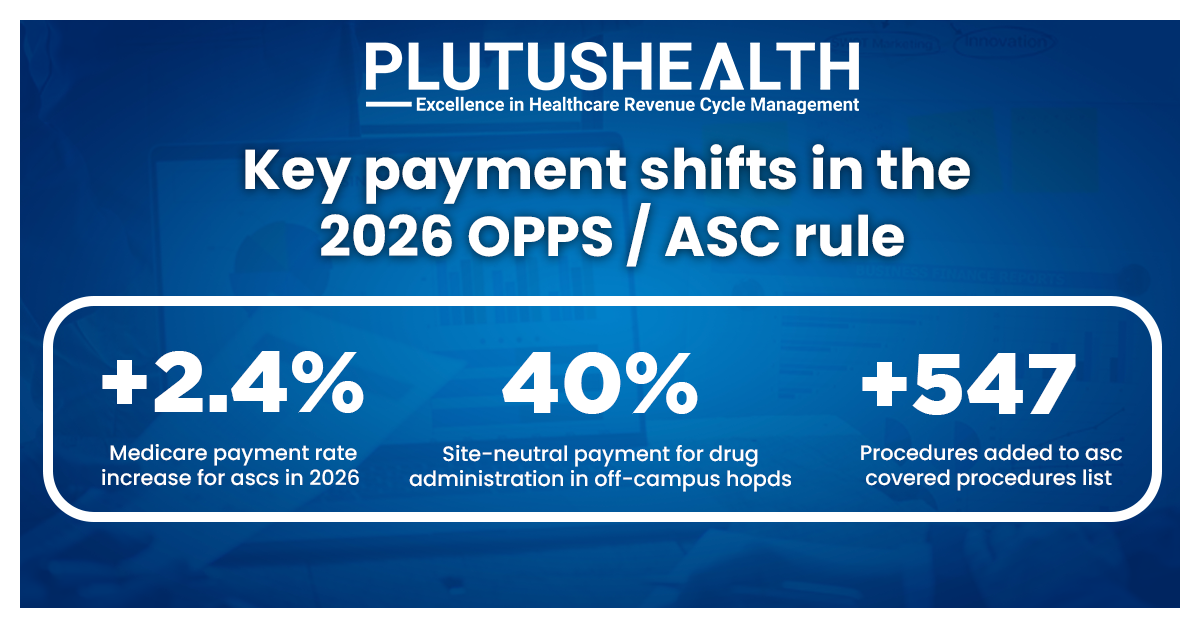
Under the proposed rule, Medicare ASC payment rates will rise by 2.4% in 2026 - matching the hospital outpatient rate increase. This stems from a 3.2% market basket update minus a 0.8% productivity adjustment.
On the surface, this is good. But inflation in medical supplies, personnel, and surgical devices has always outgrown reimbursement increases. The growth might stop further margin loss, but it won't necessarily generate new profits.
Key caveat: ASCs will only receive the full increase if they meet ASC Quality Reporting Program (ASCQR) requirements, a compliance area requiring consistent investment. Our best takeaway from the scenario is to build your 2026 budget using true cost projections, not just CMS's 2.4% rate. Align quality reporting compliance with operational efficiency to secure full payment eligibility.
Site-Neutral Payments: Shifting Competitive Dynamics
CMS keeps pushing site-neutral payment policies forward, narrowing the reimbursement difference between ASCs and hospital outpatient departments (HOPDs). Beginning in 2026, off-campus HOPD drug administration services will be paid 40% of OPPS rates, consistent with levels under the Physician Fee Schedule.
Though this affects hospitals more, it reinforces the ASC value proposition - higher-quality surgical care at a lower cost.
CFO takeaway: Leverage site-neutral policy changes in payer negotiations. Position your ASC as a cost-efficient, equally effective alternative for an expanded range of outpatient procedures.
Strategic Actions for ASC Leaders in 2026
1. Seize Growth from New Procedures
- Focus on high-margin cases that fit your existing clinical capabilities.
- Engage surgeons and care teams early to build smooth workflows for new service lines.
2. Preserve Margins Through ASC RCM Automation
- High-acuity cases mean more documentation, coding, and claims complexity.
- Use automated eligibility checks, coding validation, and claims scrubbing to maintain 95%+ clean claim rates. Plutus Health's ASC-focused RCM solutions are designed to support these goals.
3. Build Stronger Payer Relationships
- Leverage site-neutral policy changes as negotiation tools for better rates.
- Use measurable data - such as your ASC's safety record, efficiency metrics, and patient satisfaction scores to strengthen your position with commercial payers.
4. Optimize Quality Reporting and Compliance
- Meeting ASCQR requirements is essential to receive the full 2.4% rate increase in 2026.
- Implement processes that integrate quality reporting into daily operations to avoid compliance becoming an added burden. Plutus Health can streamline these reporting workflows within your revenue cycle.
5. Strengthen Financial Forecasting and Cost Control
- Model the financial impact of new procedures, staffing needs, and equipment investments before committing to service-line expansion.
- Track your cost-to-collect and A/R trends monthly to spot risks early and keep margins healthy.
As the 2026 OPPS/ASC Proposed Rule redefines the future of surgical care, success will come to ASCs that can embrace rapid change, grow smart, and maintain margins while performing increasingly complex, higher-value procedures. Plutus Health offers ASC-focused organizations exclusive RCM services, which combine automation, compliance know-how, and real-time analytics to enable CFOs to unlock the complete value of CMS's payment migration.
From prevention of denial to claims scrubbing and eligibility verification to clean claim optimization, our solutions are crafted to provide 95%+ clean claim rates, accelerated reimbursements, and improved payer relationships.
Schedule a No-Obligation Call with Plutus Health today and discover how we can future-proof your ASC's margins and operational efficiency in 2026.