Finding the Balance: Hybrid RCM Models for Behavioral Health Practices
In today's healthcare scenario, Behavioral Health practices face one of the most complex billing landscapes, as the parameter isn't about just one payer type or policy change: it's a whole new era of multiple payer types, frequent policy changes, and sensitivity of behavioral health services. All these converge into a giant parameter that organizations need to be aware of to create a healthy revenue cycle management structure.
For many years, organizations have had two standard options when it comes to billing – either completely keeping it in-house and stretching the current administration thin or fully outsourcing and placing their trust in new hands. However, recent developments have emerged, where providers are keen on exploring a new option, much like the way we work in our personal lives: the Hybrid RCM Model.
Hybrid, as the word says, is an adaptable approach in any condition. This approach combines internal staff strengths with outsourced expertise, striking a balance between control, flexibility, and efficiency. In this blog, we'll explore what makes behavioral health billing different from other specialties, how a hybrid RCM model works, and how we can help behavioral health organizations make the shift without disruption of continuous care.
Why Behavioral Health Billing Is Unique
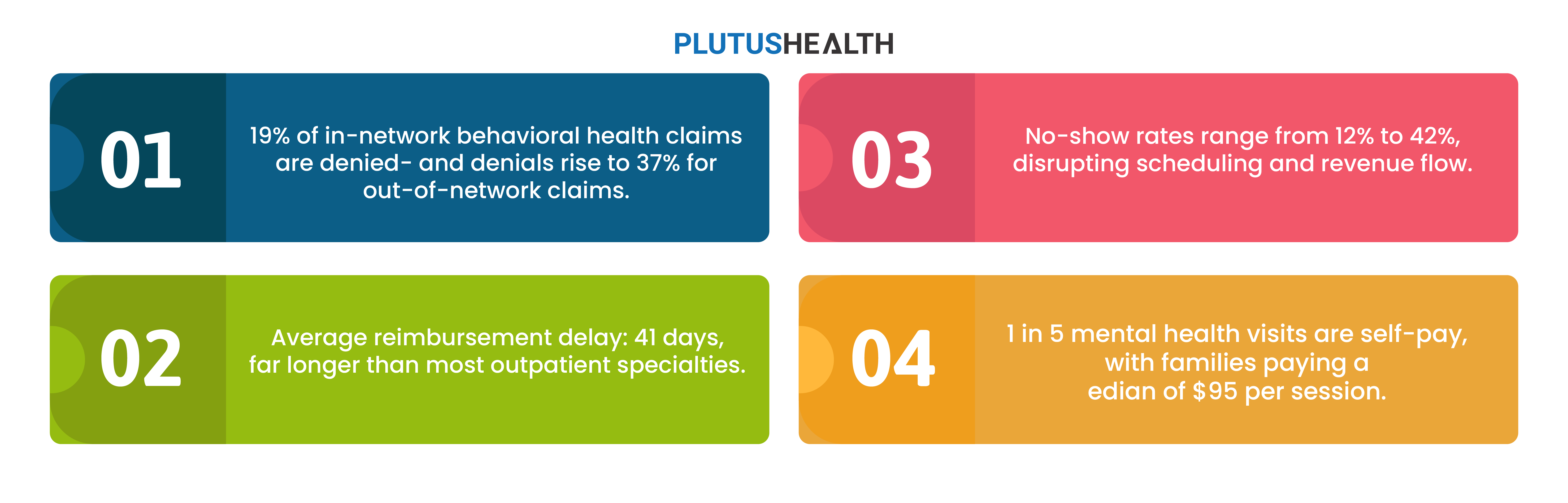
Behavioral health billing comes with a few rare challenges:
- Constant payer rule changes: CPT codes, modifiers, and telehealth policies shift frequently.
- Session length variations: Therapy sessions aren't often recorded at a set time. These vary from 15-, 30-, 45-, or 60-minute therapy sessions, which can complicate coding accuracy.
- High no-show rates: When patients fail to attend their appointments, it causes chaos, leading to authorization and reimbursement issues.
- Patient sensitivity: Compassion is key in this profession, as behavioral health providers need to balance billing or collection efforts; often, in such situations, health requires a higher degree of compassion.
- Greater reliance on self-pay and HDHPs: When patients are responsible for their own financial commitments, it becomes a bit more complicated for providers to get the complete collection.
What Is a Hybrid RCM Model?
A hybrid RCM model is a combination of using our internal resources' strengths and combining with an outsourced billing expertise to create a balanced and efficient revenue cycle.
In-house teams focus on front-end tasks, such as patient intake, eligibility checks, and scheduling appointments. Outsourced experts can handle the complicated backend tasks that demand technical precision, scale, and specialized knowledge.
This model ensures that practices maintain control of patient interactions within their buildings, fostering strong patient engagement, while benefiting from advanced billing tools, automation, and denial management capabilities.
What to Keep In-House (Front-End Tasks)
Behavioral health practices benefit from keeping patient-facing functions under their direct control, including:
- Patient intake & demographics – In-house teams are definitely required for this task, as patients can become more familiar with them and feel comfortable enough to ask them anything.
- Eligibility verification – While automation can assist with this process, having an in-house team member can reduce the risk of duplication and ensure accurate authentication.
- Copay collections – Having a variety of payment collection methods familiar to both organizations and patients benefits both parties.
- Session documentation – Continuity of care is assured when familiar faces are present in each session, who can document the process as needed.
- Patient scheduling & communication – The internal team should handle appointments and engagement to ensure familiarity and build trust amongst the patients.
These tasks rely on trust, continuity, and familiarity with the provider. Patients are more likely to engage when communication comes directly from their care team.
What to Outsource (Backend Tasks)
This is where Plutus Health helps behavioral health practices maximize efficiency. Plutus Health has an all-outsource model, which can help providers take a sigh of relief, as we have more than 18 years of experience handling the complete RCM roster.
- Claim Scrubbing & Submission: Any error in the claim is rectified before submission, and it is cross-checked through an automated claim status verification algorithm. We act as an intermediary between providers and insurance companies, thereby simplifying the billing process.
- Denial Management and Appeals: AI integration, along with our RPA bot Zeus, is used to rework denials, and our specialists work around the clock to reduce A/R aging.
- Payment Posting and Reconciliation: An automated system tracks payer and patient payments accurately and instantly.
- AR Follow-Up and Patient Statements: Smart workflows actually prioritize accounts by risk to enhance collections.
- Reporting and Analytics: Centralized dashboards provide the C-suite audience with visibility into Days in A/R, NCR, denial rates, and patient engagement.
By outsourcing these complex functions, practices free their staff to focus on patient care.
Benefits of the Hybrid Model
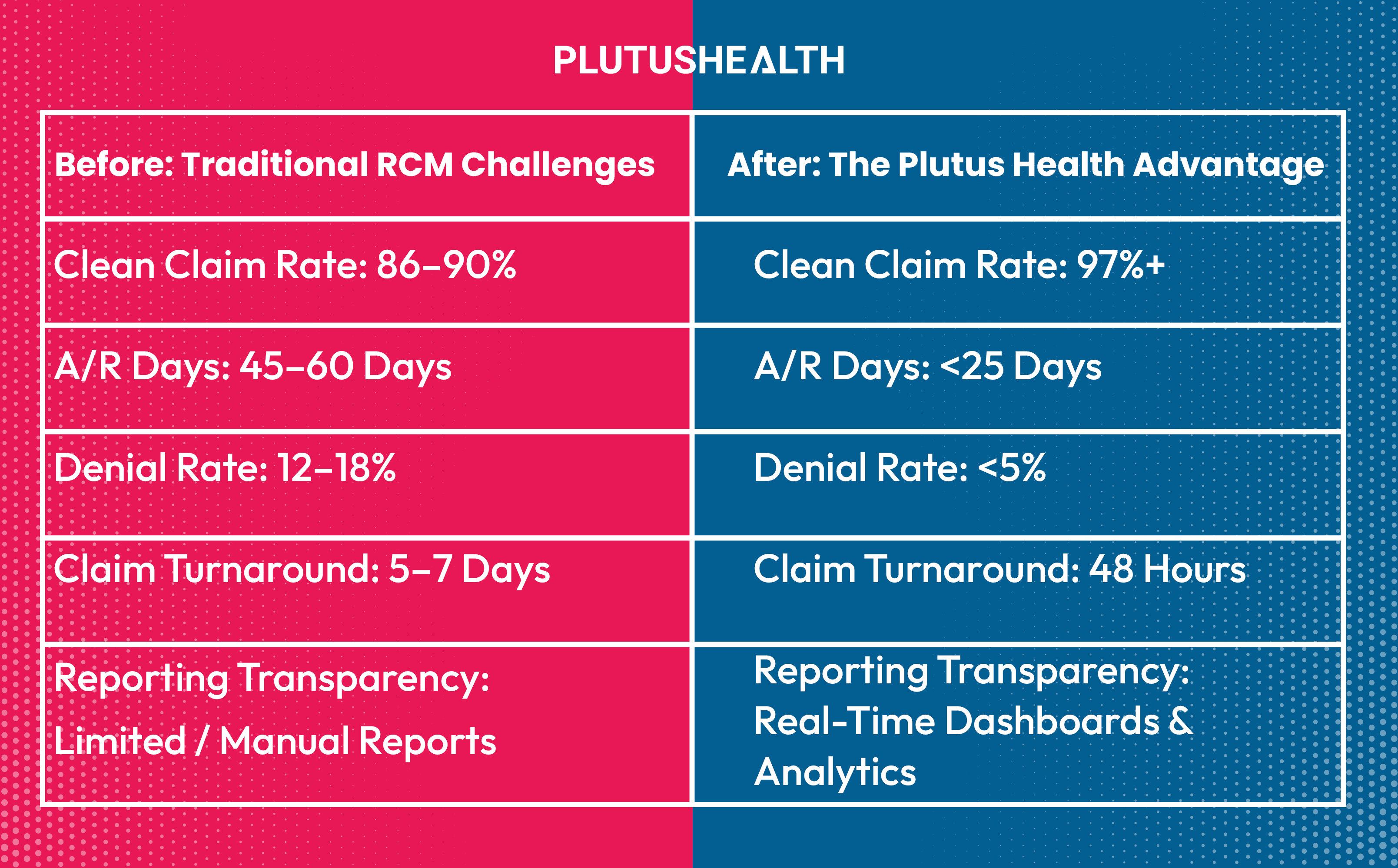
With respect to financial results and improved operations, measuring the impact of adopting a hybrid model works as follows:
- More control: Manage your patient communication directly and let us handle the technical work.
- Easy to scale: Back office staff can be increased without the need to recruit, train, and supervise additional billing personnel.
- Improved cash flow: Clean claims and quick collections lead to better financial outcomes.
- Greater agility: Changes in payer policies and patient volumes can be easily and quickly accommodated.
- Regulatory compliance: Corporate partners handle the billing in a manner that keeps compliance with the latest regulations
How Plutus Health Enables Hybrid RCM for Behavioral Health
Plutus Health partners with behavioral health organizations, including psychiatrists, SUD Practices, psychologists, therapy groups, and integrated behavioral health systems, to make hybrid RCM seamless.
One large behavioral health network of hospitals working with Plutus reduced their AR days from 90+ to 25, all while increasing staff productivity and patient satisfaction.
Key Considerations Before Making the Shift
Before transitioning to a hybrid RCM model, leaders should:
- Assess team capacity: Which tasks can your current staff perform reliably?
- Identify weak links: Where are denials, delays, or errors most common?
- Select the right partner: Choose an RCM vendor with proven behavioral health expertise.
- Ensure integration & transparency: Shared dashboards and communication channels keep your team informed and in control.
In behavioral health, efficiency and compassion must coexist. A hybrid RCM model provides organizations with the control they need, while also addressing the efficiency they lack, enabling them to balance patient care with financial sustainability.
Let's Talk Hybrid RCM.
Book a free assessment with Plutus Health today and learn how we can help your behavioral health practice cut costs, improve collections, and focus more on patient outcomes.