The Future of Healthcare Payments: Empowering Patients & Sustaining Providers
The modes of patient payments have evolved significantly since the days of only cash transactions. For decades, billing was treated as a back-office process, important, yes, but far removed from the clinical and human side of medicine. That era is over.
The moment a patient receives an unexpected invoice, their lack of understanding of the options forces them to make a financial decision, and the psychological effect of that event is not limited to mere revenue; it also affects their trust in the care they have received. On the other hand, healthcare providers are in a situation where they cannot ignore the growing pile of bad debts, increasing denials, and the ongoing shift from fee-for-service models that are becoming less important.
The problem that healthcare top management has to deal with is straightforward: how to build a payment ecosystem that empowers patients, leverages healthcare payment technology, and ensures long-term financial sustainability? The future of healthcare payments won’t be won by those who chase transactions. It will be led by those who align financial clarity with clinical excellence.
Patients Want Empowerment, Not Confusion
One of the most notable shifts in recent years is the way patients perceive their role in the financial aspect of care. They are no longer just waiting for the bills to come; they have taken the role of healthcare consumers. They check the prices, make comparisons among the different doctors, and ask for the same openness that is given to them when booking a flight or paying for groceries. A poll conducted by the Medical Group Management Association found that 94% of Americans support greater price transparency in healthcare services. This is not merely a wish; it is a must.
Medical practices that provide real time cost estimates and offer installment payment plans have seen a 10% or more increase in collections, alongside increased patient satisfaction.
Think about it: a patient who gets a complex bill weeks after the treatment feels totally perplexed. On the other hand, a patient who is given a clear estimate beforehand, accompanied by the option to pay gradually, feels honored and empowered.
For leaders, the lesson is simple: financial empowerment builds clinical loyalty. When patients trust you with their wallet, they’ll trust you with their health.
Technology Is Rewriting the Rules
Transparency alone is not enough. Delivering it at scale requires technology that can simplify complexity and anticipate financial friction before it happens. That’s where AI in healthcare billing, automation, and digital payments are transforming the game.
Predictive analytics now scan patient and payer data to flag claims likely to be denied before they are even submitted. By addressing errors upfront, providers can reduce denials by up to 20%, according to industry studies. Digital wallets, mobile payment apps, and online patient payment solutions, once seen as retail luxuries, are now mainstream in healthcare. In fact, 94% of organizations using digital payment tools report faster collections and happier patients (Kubra).
But the most exciting frontier is AI-driven personalization. Picture a scenario where a payment is not only processed but also a personalized financial plan is created specifically for a patient based on their individual characteristics, including medical history, risks, and even their preferred method of communication. This is a dream of the future, but it has already become a reality. For the managers, the most important point is very simple: technology has transformed from being a cost center at the back end to a front-end powerhouse in revenue cycle management.
The Human Edge Can’t Be Automated
And make no mistake - the human touch still matters. Patients need assurance and guidance when making the most important decisions of their lives, and they do not want to discuss it with a chatbot, which wouldn’t share the empathetic feelings of a healthcare provider.
Financial advocates, who have usually been a part of the healthcare system, are now considered as important as medical professionals. They clarify the connection between the complicated billing procedures and the personal experiences related to them. They support families in coping with insurance, discuss various payment options, and bring compassion during the most challenging moments.
For C-suite leaders, the strategic move is not choosing between technology and people; it’s blending the two.
Automation is powerful, but empathy is irreplaceable. Let AI handle repetitive tasks, freeing your advocates to do what only humans can: build trust.
Payment Models Are Evolving—Are You Ready?
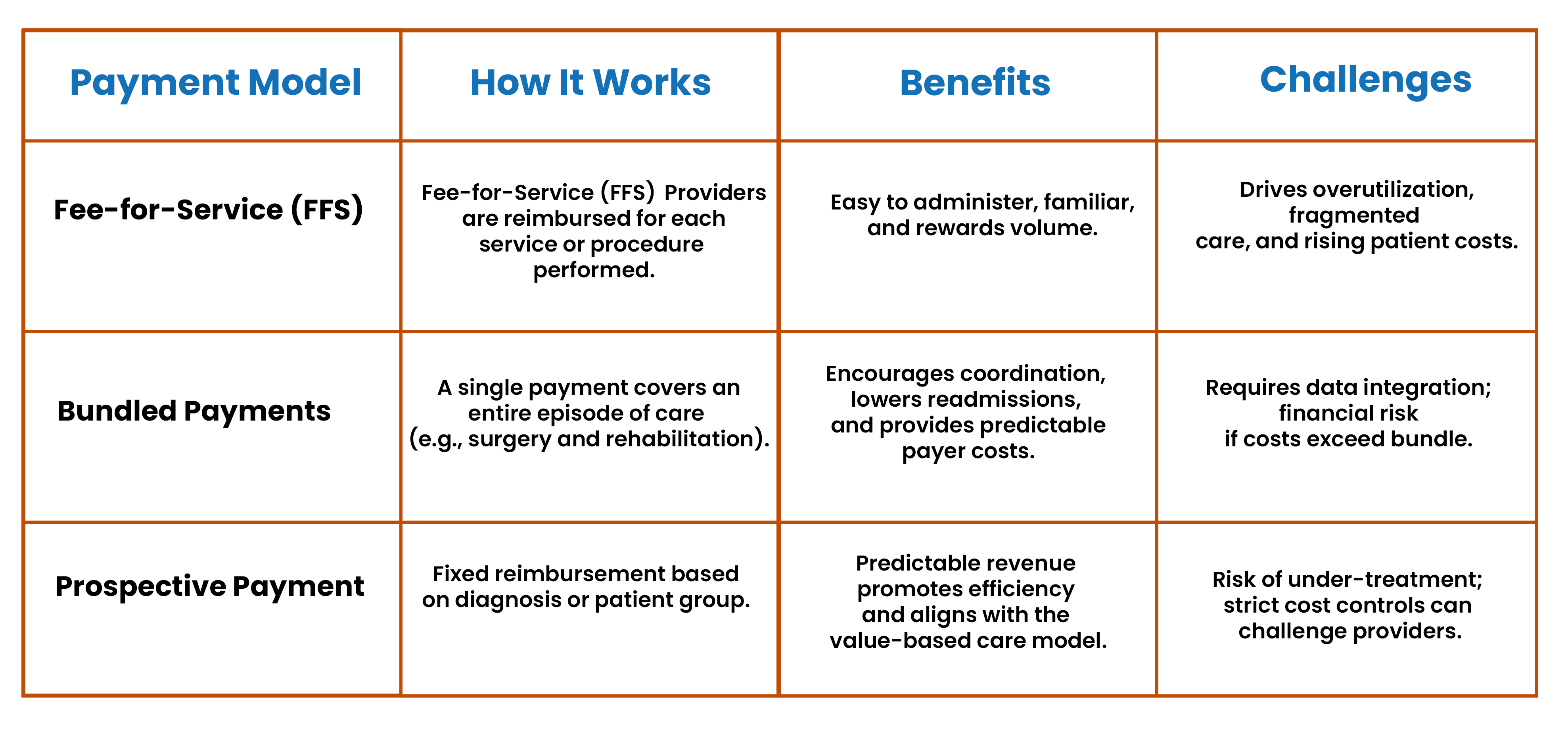
While patient empowerment and technology are reshaping the front end of payments, systemic changes are transforming the back end of the healthcare system. The dominance of fee-for-service is waning as bundled and prospective payment systems take center stage.
Here’s a quick look at what’s at stake:
Bundled payments reward collaboration and can reduce total costs without compromising outcomes. Prospective systems offer predictability but demand discipline. Each model comes with trade-offs, but they share a common thread: aligning financial incentives with quality of care.
For executives, the urgency is real. Whether mandated by payers or chosen strategically, payment reform is accelerating. Organizations that prepare now will be in control of their destiny. Those who wait will be forced to adapt on someone else’s terms.
The Plutus Health Approach
At Plutus Health, we view the payment process as an integrated journey, rather than a segmented one, an aspect that involves the participation of every stakeholder, from patients and providers to payers. Our philosophy is a combination of three commitments:
- Patients will be empowered through precise estimates, adaptable financing, and open billing.
- Providers will be made capable through AI-driven denial prevention, predictive analytics, and digital-first payment tools.
- Human role will be enhanced as advocates supporting patients through financial stress with compassion and expertise will be empowered.
We also assist healthcare organizations with our patient payment system, AnodynePay, which provides a seamless digital payment platform for both patients and providers. In other words, we don’t just manage revenue cycles; we build payment ecosystems that last.
Looking Ahead
For top executives, it is a tough but clear way ahead. Make every interaction of the patient with the hospital or doctor transparent. Allocate resources for AI and digital payment tools that will increase both efficiency and personalized service simultaneously.
The winners will not be the ones who chase every new tool or cling to old ways of working. They will be the ones who combine technology with empathy, match financial goals with patient needs, and consider payments as an integral part of the care process. At Plutus Health, we believe the future of healthcare payments is not about choosing between people and profits but proving that you can serve both.